The Pandemic, General Practice, Doctor Shortages and Burn Out
Whether we like it or not, we are in the 3rd and 4th wave of the Pandemic, and things have pretty much progressed as expected.
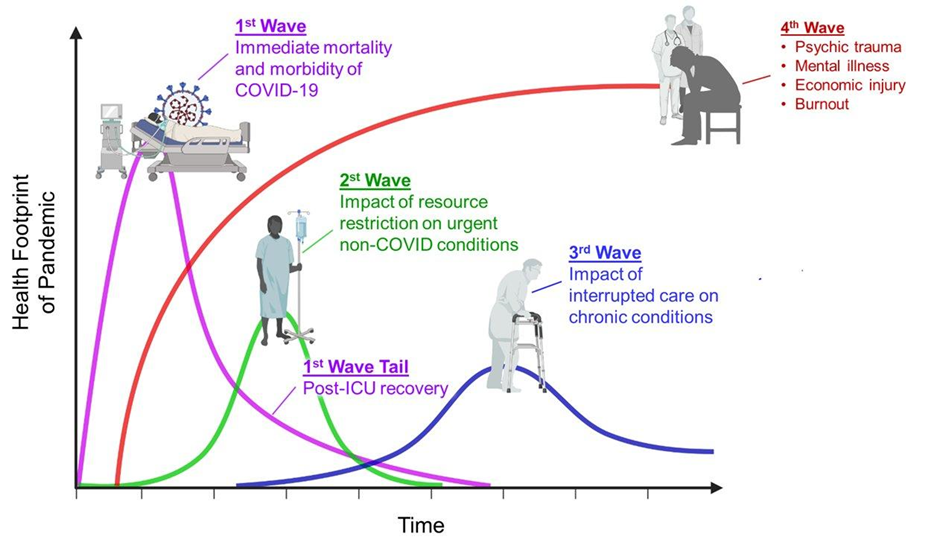
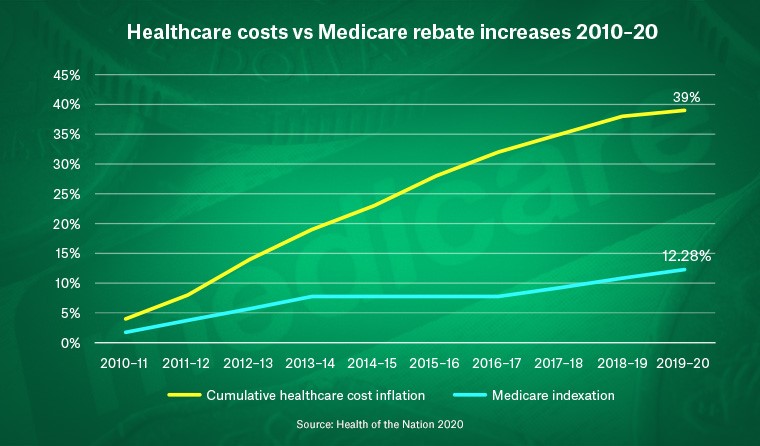
At the Primary care level, we as GPs are feeling the pressure. We are feeling the impact of the interruption on chronic care, and the mental health caseload has exploded. Many health professionals are exhausted and burnt out. Successive governments have not increased the Medicare rebates to keep up with the health care costs. We have been asked to bulk bill all telehealth, and Covid vaccines, which we have all done as our patients have needed us. But our significant pressure now is that there are not enough GPs on the ground to do the work required.
The failure of workforce policy
Immigration has all but ceased, and junior doctors are fleeing the profession for the safe haven of well-paid specialist jobs where they won’t be forced to go and train rurally. Paradoxically the smaller towns have done well from both District Priority Area (DPA) (limits the areas international medical graduates can work in) and Rural Bonding (Australian students’ scholarships in return for rural time as a professional) has forced doctors to go further and further from the cities, but this will only last a short time as doctors are not seeing enough patients and are not getting the support and training they need in the smaller and most remote towns, so inevitably they will bounce back to the safe haven of the city.
In theory, both things should work well, and the reality is they do not. Both groups generally do the minimum number of hours and years and return to the city as soon as possible.
So, all in all, those of us who are left providing services in regional and outer metropolitan areas are exhausted – our communities are not small enough to qualify for District Priority Area (DPA) or attract Rural Bonded Australian graduates.
The failure of Medicare rebates to keep pace with inflation makes General Practice less attractive for medical graduates with only 15% of graduates opting to become GPs.
The reality for regional centres and outer metropolitan areas is that we are entirely dependent on immigration to fill vacancies in Primary care. In order to continue to provide services, we need a review of the DPA system to allow immigration to occur again. If we had access to more Doctors in Primary Care, there would be less pressure on the much more expensive option – Tertiary care.
We already have the infrastructure in primary care – what we need is the ability to recruit and the ability to pay GPs properly; both things rely on two things: –
- A review of the failing workforce policy.
- Medicare rebates keeping up with inflation/actual cost of health care.
Prevention is better than cure. Primary Care is far cheaper than Tertiary Care, but we can’t provide services if we can’t recruit and retain GPs.
DPA is due for its first full review in three years in July, now is the time to speak with your Member of Parliament about the issues facing General Practice
Dr Brenda Murrison
Founder and CEO Brecken Health Group, WA; AGPA Director
MBChB DRCOG MRCGP FRACGP GAICD MBA


Leave a Reply
Want to join the discussion?Feel free to contribute!