General Practice is on the edge of a cliff and has been put there by the actions of Successive Governments.
There are three key components to a high quality primary healthcare system
- Professionals- Sufficient well trained and appropriately remunerated staff including GPs, Nurses, Allied Health Professionals and Administration staff,
- Practices – High quality infrastructure provided by GP Practices with up to date standards and facilities, and
- Patient Access- Ease of patient access which is impacted by cost of access, timeliness of access, and the transportability of access (competition between GP Practices)
Most GPs work in Principal led (GP Owned) Practices, small businesses that are the backbone of Australia’s primary health care system. These General Practice businesses are under extreme pressure. The Australian GP Alliance (AGPA ) is the representative body for GP owned practices which account for over 2/3 of General Practices (ref HON 2022).
We call on the Federal Health Minister to act in this time of crisis to for Primary Health Care in Australia.
Fundamentally the health of all Australian citizens is under threat as their access to high quality, universal health care is in jeopardy.
Patient access has been undermined by policy decisions taken by successive Federal Governments advised by the Department of Health. By sustained freezing of the Medicare rebate, the Federal Government has stripped support for Australian’s health and in turn reduced funding to General Practice. During this time GPs and Practice Owners underwrote access to primary care by accepting reduced rebates as payment which in turn stifled GP and practice income. This is no longer sustainable. Australian GPs receive approximately 2/3 of the salary equivalent of OECD primary care specialists (HON 2022).
Doctors in training are aware of the pressures in General Practice and are refusing to enter a specialty which offers considerably lower remuneration than other specialties and an immense red-tape burden. Practices are no longer able to “bulk bill” vulnerable patients and many are now barely financially viable businesses.
Below we outline key factors which must be urgently addressed in order to rescue General Practice from collapse and thereby protect patient access to our world class health system.
Practice Costs have been rising while revenue has been falling
Staff Costs
Reception staff have been an integral part of our response to the pandemic. They are exhausted and burned out. Many are leaving the industry, leading to recruitment problems for practices. Demand for replacement staff in a time of labour scarcity has driven up wages considerably. A 5.2% rise in the minimum wage has increased the cost associated with tied awards, as well as increasing staff expectations. Since public sector Health Administration staff are paid considerably more, by virtue of adequate funding, retaining General Practice staff has been very difficult.
General Practice nursing wages have been increasing by 8% per year since 2016 but still fall considerably short (by 20-30%) of public sector Health and vaccination hubs. Nurses stay in General Practice for the culture and the rewarding work but are being disadvantaged by the lack of appropriate funding support for General Practices to employ nurses and perverse MBS requirements. Government workforce incentives for nurses in General Practice are inadequate, capped and have never been indexed.
Service costs
Electricity costs in most jurisdictions have increased by 10% or more in 2022. Almost every service used by General Practice have increased their costs in line with headline inflation or greater, which is more than 6%.
Medical supplies have increased in price in the order of 10% per annum over the last 2-3 years.
Greater demands for equipment to manage the COVID pandemic – such as personal protective equipment (PPE), cleaning products and physical barriers and signage have been a major cost onslaught.
General Practice Revenue has been falling in real terms due to inadequate Government support
Service fees of doctors and other health professionals are heavily influenced by patient capacity to pay which is inextricably linked to Medicare rebates. These have been going backwards in real terms. No industry can be expected to survive falling real revenues. General Practice is no different. The viability of practices is in peril.
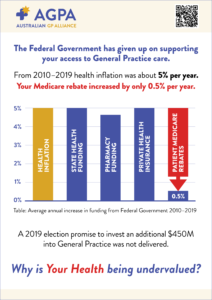
Given that on average Medicare rebates have risen by 0.5% per annum over 10 years and health inflation is ~ 5% per annum, estimates suggest there has been a 35 to 50% reduction in real practice income over 10 years.
Government support payments such as Practice Incentive Payments and Workforce incentives are not indexed. The funding parcel is capped. In real terms, noting health inflation of ~ 5%, Government funding to General Practices, has fallen by between 35 to 50% in real terms over 10 years.
As a result of these policy settings the community is suffering.
There has been a 6% decline in the number of General Practitioners in the last 18 months. 7500 GPs plan to retire in the next 5 years. Only 13.8% of medical students plan to train in General Practice. 1350 GPs are trained every year by the RACGP. There will be a ~ 30% gap, some 10 000 GPs, between the demand/need for GPs and the supply by 2032. Wait times to see a GP are climbing. Emergency Department presentations are growing – at a cost to Government of 15-20 times the cost of GP care. Providing accessable care for disadvantaged patients, with no out of pocket costs, is becoming unviable for Practices and unavailable to patients as bulk billing falls at a record pace as Government underfunding forces Practices to increase prices to survive.
We need to support a burned out workforce who has supported the community through this pandemic
AGPA calls for the Labor Federal Government to act urgently in this emergency situation. General Practice has provided more than 60% of all COVID vaccinations coping with a haphazard, tortuous Government led “stroll out”. We have supported patients while hospital outpatients were closed and avoidance of hospital situations was desirable. In the midst of a pandemic, we have managed respiratory illnesses and other presentations of people with possible viral illnesses in a manner which is safe for our patients and staff. Practices had to fund safety measures such as PPE and equipment such as HEPA filters with little support from Government.
While States such as Victoria and NSW gave pandemic bonuses to all of their health administration and health workforce, General Practice receptionists and nurses got no such acknowledgement. Violence against health care workers (HCW) is legislated with mandatory sentencing in many jurisdictions but GPs and their staff are often not included in these definitions of HCW. Verbal abuse and antagonism towards our reception and nursing staff has been prolific. These staff are the backbone of General Practice and deserve better.
We call on the Federal Government to:
- Immediately provide funding to support Nurse retention in General Practice by providing one off emergency Workforce incentive payments and improving long-term support before the end of 2022.
This will allow General Practices to retain their nursing workforce which has provided 60% of Australia’s COVID vaccinations. Nurses want to stay in General Practice but have the same cost of living pressures as everyone else and are entitled to a fair wage.
- Immediately commit to developing workforce training and retention packages for nurses to act in their full potential within a General Practice team.
Practice nurses should be supported to provide care within their scope of practice supported by the wider General Practice team. The Federal Government should create Medicare items for nurse led wound care, immunisations and health care coordination within a General Practice. Some of these existed before Medicare cuts were made. Nurse and reception salaries need to have parity with State Health if we are to have any hope of retaining these staff.
- Immediately reverse the underfunding of General Practice that occurred during the “Medicare Rebate Freeze” era and commence the establishment of an independent pricing authority for all health care to ensure government investment is evidence based.The 2008/2009 Health and Hospital reform commission report led to both an independent hospital pricing authority which set an “efficient price” (ihacpa.gov.au ) and a national performance authority (now brought in to the Australian Institute of Health and Welfare). AGPA calls for the establishment of an independent pricing authority for the MBS so that an efficient price for out-of-hospital care can be set, and the pricing of MBS items can be moved away from the political whims of Government.
- Adjust the Medicare Safety net and Enhanced safety net provisions
Ease the impact of cost of patient access by initially reducing the threshold to access the Medicare safety net and enhanced safety net along the lines of the reduced co-payment for PBS prescriptions.
Merge the MBS and PBS safety nets so that patients only have one threshold to pass over before qualifying for the safety net provisions. This will support patients with high needs such as the elderly to access care where and when they need it.
- Invite Practice Owners to the Reforming Medicare Taskforce
Listen to those who run the General Practices of Australia – the GPs who are owners and practice managers. The Australian GP Alliance, as the representative of GPs who own and work in practices, should have a seat at the table and be part of planning our way out of this mess.
With the collective experience of hundreds of GPs who have built, grown and sustained General Practices for ‘purpose above profit’ we bring a wealth of knowledge of how to meaningfully reform policy for the benefit of our patients and communities.
We must be careful not to lose the best of our world class health care system. Emulating overseas funding models which provide inferior care and outcomes is not in the best interests of the Australian community.
Creating a thriving General Practice sectors saves money, reduces the burden on the emergency and hospital sector, improves patient access to healthcare and most importantly improves health outcomes. The evidence for this is indisputable. The Federal Government needs to act now before it is too late.