NZ: reducing GP fees not so simple

In the recent New Zealand election campaign, one policy united parties from all parts of the political spectrum – their intention to reduce the fees patients pay for GP practice services. The only difference was by how much fees were promised to fall and which groups within the community would benefit from increased subsidies.
However, it is not a simple matter for a political party to promise that increased government subsidies will lead to fees falling by an identical amount at all practices. This is because, since the New Zealand Primary Health Care Strategy (NZPHCS) was introduced in 2001, GPs are no longer paid an exact subsidy for each consultation. Instead, they are paid for each patient enrolled. The fees charged at each practice will therefore depend on the number of consultations delivered.
To illustrate (see Table 1), assume that two hypothetical practices, A and B, each have an identical number and type of patients enrolled and are identical in all other respects. Each receives the same amount of funding from the government ($250,000 – simplified for this illustration), based on the assumption that on average each delivers 10,000 consultations a year. Each charges $25 per consultation. It costs on average the same for each to provide a consultation ($50, including the cost of practitioner time and all overheads).
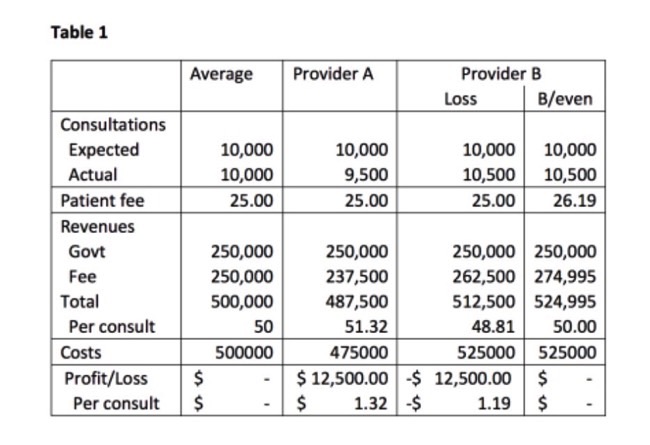
If each practice delivers exactly 10,000 consultations, it will break even. If practice A delivers 9500 consultations instead of 10,000, because it is ‘lucky’ and has healthier-than-average people enrolled, it will make a profit of $12,500. If practice B delivers 10,500 consultations, because it is ‘unlucky’ and has sicker-than-average people enrolled, it will make a loss of $12,500.
If practice B is to break even financially, it will have to charge higher fees than practice A. Alternatively, if the fee is to remain at $25, it must reduce it costs per consultation – for example, by delivering shorter consultations than practice A or by hiring less-experienced staff who can be paid lower wages.
Either way, patients at practice B end up worse off than those at both practice A and an ‘average’ practice as anticipated by the funding formula.
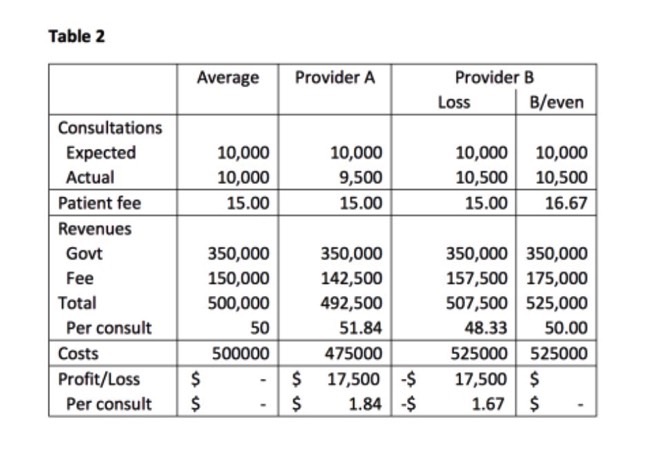
Assume now that the government wants to reduce the fee paid by patients to $15 per consultation. For an average practice, this could be achieved by increasing funding to $350,000. But, as Table 2 shows, this leads to ‘lucky’ practice A making an even larger profit and ‘unlucky’ practice B an even larger loss. If practice B is to break even now, its fees must rise by $1.67 to $16.67 (or it must reduce service quality by even more than under the subsidies paid in Table 1). All patients pay a lower fee, but those at practice B face an even greater disadvantage now compared with both practice A and the average practice.
Tables 1 and 2 illustrate the perverse outcomes arising from subsidy arrangements under the NZPHCS. The policy has led to an inequitable outcome between patients at different practices facing different utilisation rates for reasons that cannot be anticipated in the funding formulae.
The reason is that government funding payments are in effect an insurance premium, paid in advance (it is called a ‘prospective’ payment) for the expected care needs of people enrolled at a GP practice. Payments are the same regardless of whether the practice is ‘lucky’ and delivers fewer consultations than expected or ‘unlucky’ and delivers more.
The difference between the expected and actual number of consultations leads to a financial risk borne in the first instance by GP practices.
In New Zealand, the government pays only part of the costs of primary care and practices have historically charged patients the difference.
These patient payments are ‘retrospective’, levied after a consultation has taken place. They allow practices to pass on financial risk resulting from any shortfalls because of the funding formulae. The higher the share of income practices receive from the government, the greater the financial risk they face, and the greater the shortfall passed on in patient fees (or service quality reductions) at ‘unlucky’ practices.
If the government wants to reduce patient fees, but not increase the financial risk faced by practices and patients, the additional subsidy to reduce fees further should be a retrospective one per consultation actually delivered and not a prospective one per number of patients enrolled.
Table 3 shows that if, instead of increasing the prospective funding from $250,000 to $350,000, the government instead paid a retrospective fee of $10 for each consultation delivered (in similar fashion to before the NZPHCS), patient fees would fall by $10 and the outcome for each practice would be the same as in Table 1.
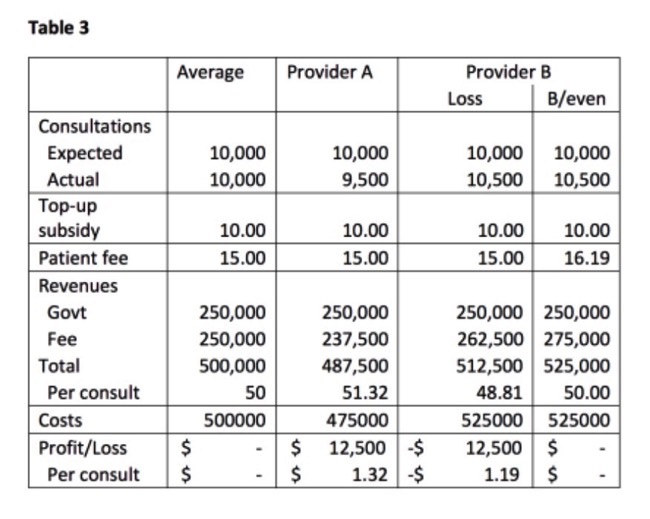
This “mixed payment method arrangement” does not remove inequities between the ‘lucky’ and ‘unlucky’ practices, but nor does it make the comparative disadvantage greater.
If making additional subsidies to reduce fees retrospective reduces inequities, would making all government funding paid to GPs retrospective be even fairer still?
Unfortunately, this is not an ideal situation either, as it discourages primary care providers from allocating sufficient time and other resources to valuable activities other than consultations – for example, collegial interactions with other providers within the local Primary Health Organisation (PHO) to devise and implement care programmes that raise the health of the whole PHO population.
The key is for government subsidy payments to be made in a manner that minimises the financial risks faced by each of the government, providers and patients at the same time as encouraging the most efficient use of the limited funding, time and other resources available.
To paraphrase health economist James Robinson, the two worst ways of subsidising GPs are with a purely prospective or a purely retrospective payment.
A “mixed payment method” as described here blunts the rough edges by limiting the lurch from one imperfect payment system to another.
* Dr Bronwyn Howell is in the School of Management at Victoria University of Wellington.
This article first appeared in https://www.newsroom.co.nz
Leave a Reply
Want to join the discussion?Feel free to contribute!