A PDF copy of Australian GP Alliance 2022 Federal Election Statement is here
AGPA Federal Election Statement
The Australian GP Alliance (AGPA) was formed in 2016 and represents General Practice Principals – the General Practitioners who work in the Practices that they own. These are the Doctors who keep General Practices open and operating. Providing the platform that supports the Australian primary healthcare system.
The Australian General Practice Alliance believes that to ensure the long term integrity of Australia’s Primary Healthcare System the following issues must be urgently addressed:
- The immediate reversal of the underfunding of General Practice that occurred during the “Medicare Rebate Freeze” era and the establishment of an independent pricing authority for all health care to ensure government investment is evidence based.
- Reform of the management of chronic physical and mental diseases by encouraging the voluntary registration of patients for provision of chronic care while maintaining ease of access and patient choice by retaining Fee For Service (FFS) for episodic care.
- Modernisation of healthcare delivery to improve convenience and ease of access by making existing Telehealth rebates permanent in a way that supports patient choice.
Our Concerns
Australia enjoys one of the best Primary Healthcare systems in the world centred on General Practice. There are clear signs that this system is under significant stress and without clear and determined attention from the Australian Government this high quality system will decline. Australians will lose local, accessible, affordable personalised care supporting them through illness and robust health.
A significant decline in the quality of and access to Primary Healthcare will delay the provision of medical care for Australians. This will place further pressure on the whole health system and in particular hospital services – resulting in increased waiting times, delays in time critical interventions and treatment, poorer health outcomes and higher health and social care costs.
As the Australian population ages, the increasing chronic disease burden is the most significant healthcare need to address. The under-resourced mental healthcare system has seen its caseload considerably increased due to the COVID pandemic. General Practice and the Primary Healthcare system are best placed to treat seniors, address chronic disease and treat and support mental health. Managing these within the community would allow more acute, severe or complicated care to be managed within the hospital system. This demands significant investment now. Without proper funding, the ability and capacity of General Practice will not be able to be realised, and neither the Primary Healthcare system nor the hospital system will be able to cope with the increasing pressure.
The importance of General Practice
General Practices provide the infrastructure which allows Australians to receive the world class Primary Healthcare they have come to expect. These Practices are largely privately owned and the vast majority are small to medium sized enterprises.
Decline in the effectiveness of General Practice in providing primary healthcare will see a long-term rise in the cost of healthcare as untreated chronic disease increase and presentations at hospitals become the method for accessing healthcare for more Australians.
The great majority of General Practitioners in Australia work as contractors relying on the infrastructure provided by the Practices to allow them to practice.
The Australian Primary Healthcare system relies on the viability of these small to medium enterprises as much as it relies upon there being adequate numbers of well qualified and dedicated General Practitioners, Nurses and other Allied Health Professionals and administrative and support staff. Similarly, the health outcomes of Australians are reliant on them having affordable and rapid access to quality health advice that they trust. If any side of this triangle of:
- high quality Primary Health infrastructure (provided by General Practices),
- high quality well trained and dedicated Primary Health professionals and
- affordable, trusted and easy access for patients;
falters or fails, then the health of Australians will decline and the cost of healthcare will significantly increase.
The maintenance of all sides of this triangle – people, infrastructure and access are key to the success of the Australian Primary Healthcare system.
We submit the following points regarding the current state of the Australian Primary Healthcare system.
- General Practice is at the Heart of the Australian Health Care system – it is trusted, effective and adaptive.
- Over 80% of Australians identify a regular GP Practice, with older Australians tending to see the same GP at that Practice.
- 8% of Australians report visiting their GP at least once per year.
- Australian GPs have delivered nearly 60% of COVID vaccinations and cared for their community members during periods of lockdown, economic hardship and social upheaval.
- General Practice is unique as the largest medical small business sector and needs to be supported by policy, not disadvantaged
- General Practice accounts for less than 9% of the Australian annual health budget and from 2010 – 2019 has received less than 0.5% annual increase in funding from the Australian Government while funding to State Health systems, Pharmacy and Private Health insurance have all kept pace with the annual health inflation rate of 5%
- Over the last 10 years Healthcare costs have increased by 39% while Medicare indexation has increased by only 12.3 % over the same period. This difference is paid for by reduced viability of General Practices, reduced incomes for GPs and allied professionals, and increased costs for patients as GPs charge higher “gap” fees to some patients to cover the costs of reduced real income from bulk billed patients.
- Declining viability of General Practices makes them less attractive to new generations of Principals, threatening the stability of the sector.
- The funding of the Primary Healthcare system and General Practice over the last decade has had more to do with political expediency than seeking to support and develop the most cost-effective sector of the healthcare system
- Reductions in GP incomes in comparison to other medical specialists and the biases of medical training are creating shortages of GPs in all parts of Australia, reducing the ease of access to the Primary Healthcare System and unnecessarily increasing pressure on hospital and their emergency systems. This decline in incomes is primarily due to the Medicare freezes. This has resulted in 5000 fewer GP specialists than non-GP specialists, the inverse of what the system requires and a situation which increases health care system costs.
- Attempted substitution of GP specialists with unsupervised allied health professionals will inevitably result in reduced quality of primary care being available to Australians.
- The Medicare Fee for Service (FFS) system has served Australia very well making Primary Healthcare accessible and affordable for Australians and providing excellent outcomes.
- While there has been criticism of this FFS approach and its ability to deal with chronic disease, it is a crucial part of the system ensuring access and equity, particularly for disadvantaged communities who are more likely to frequent multiple practices for episodic care. Fee for service is the only way to guarantee access and flexibility for patients and is a fundamental part of our effective health care system.
- Statistics indicate that while Australians strongly prefer to see their “own GP” and their “own practice” this is not always possible, particularly for acute issues. However, all systems can be improved and we believe new processes could be introduced which will improve continuity of care.
- While registration of patients with a Practice or GP has potential to improve the continuity of care, it is essential that this is predicated on new funding and is structured so that it:
- is voluntary and underpinned by a commitment to patient centred care including ensuring high levels of patient empowerment and agency
- does not inadvertently impede access to care by failing to ensure equity of access is maintained. This is best achieved by maintaining the FFS system for episodic care while encouraging a single GP relationship for long term chronic treatment.
- has payment systems which recognise the support from Practices to GPs and the cost of this, and the contractual nature of the commercial relationship between the GP and the Practice.
- It is essential that Practice owners are specifically and separately consulted on changes which may impact on Practice contractual relationships. Recent court decisions regarding payroll tax in Victoria and NSW have the potential to make all MBS payments made to GPs part of payroll tax calculations. Incorrect design of registration payments could make this situation worse. External financial stressors such as this have increased the pressure on Practices to either fail or reduce accessibility by raising fees and increasing levels of private billing.
- The elements of the current funding model of primary health care which provide equity of access for patients and high levels of patient choice are critical to the success of the current system. It is essential that policy decisions taken in the future aim to retain patient control over their treatment (including seeing the Doctor they choose to) and do not exclude access, either by availability of access to treatment or by the cost of treatment.
On this background we make the following recommendations:
- Correct the underfunding of General Practice and establish a structured approach to future health care funding increases and funding direction by:
-
- Correcting the underfunding of General Practice that occurred during the “Medicare Rebate Freeze” by restoring the funding levels to where they would have been without the “freeze”, and,
- Establishing an independent pricing authority for all health care so that investment in primary care, like hospital care, can be evidence based and costs can be managed more appropriately.
- Reform the management of chronic physical and mental diseases by encouraging voluntary registration of patients for the provision of chronic care (and in particular chronic care planning) while maintaining FFS funding for episodic care.
- When developing patient registration systems it is critical that Patient equity is maintained by allowing easy transfer of registration and access to alternate GPs (and Practices) for episodic care in a manner which is convenient for patients and facilitates timely and equitable access to Primary Healthcare.
- Voluntary registration must be funded to assist practices to develop effective models for working with registered patients and to train staff in new administration approaches.
- Modernise health care delivery to improve the convenience and ease of access for patients and the effectiveness of Primary Healthcare by making existing Telehealth Medicare rebates permanent in such a way as to support patient choice. Telehealth funding must not be part of any capitation or bundled payment model and patients should retain access to as needed episodic care from any GP/Practice.
Policy settings drive behaviour in health care. Health care represents a considerable expense for Government and it is in all our interests that health care policy is driven by evidence and supports care which is cost-effective and supports healthier families and communities.
It is critical for the maintenance and improvement of Australia’s world class Primary Healthcare system that policy and funding decisions are evidence based.
Background and Supporting Evidence
General Practice is at the Heart of the Australian Health Care System
General Practices have particularly intimate and meaningful relationships with all our patients, caring for young families, patients with chronic disease and the elderly.
Australians access general practice more than any other area of the health system (1) with over 87.8% of the population visiting their GP at least once each year. (3).
Australian GPs have delivered nearly 60% of COVID vaccinations and cared for their community members during periods of lockdown, economic hardship and social upheaval.
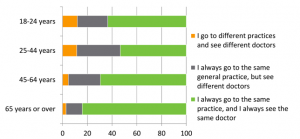
Figure 1 The majority of patients want to see their own GP/Practice. Source: Australian Digital Health Agency
Societies with mature and well-funded primary healthcare do better from a health, economic and social perspective.
General Practice is a very challenging profession if done well. GPs help manage the health needs of people, families and communities, not just illnesses and organs. They provide ‘relationship based care’ which is more effective at modifying risk factors, addressing psycho-social aspects of care and providing whole of family care (8).
It has been estimated that 5% of patients account for 50% of health care expenditure and well-resourced GPs are the solution to this problem. General Practice provides the majority of care for patients with chronic diseases and mental health issues. More than 40% of GP consultations deal with chronic diseases. This burden is set to increase considerably post-pandemic as the health system deals with late presentations of cancers, unmanaged chronic disease and new and exacerbated poor mental health including that of children, adolescents and young adults.
The post-pandemic chronic disease and mental health ‘wave/tsunami’ and the increasing chronic disease burden from an aging population will fall on a currently underfunded and understaffed Primary Healthcare system unless policies are changed.
General Practices Have Been Systematically Defunded
Most Primary Healthcare in Australia is provided via General Practices. These are generally small businesses which employ receptionists, nurses and allied health professionals, and support the local economy in the same way all small businesses do.
These Practices provide the infrastructure which allows the contractor GPs to provide the high quality Primary Healthcare that Australians enjoy. The ongoing viability of these small businesses is critical to the provision of Primary Healthcare. Their replacement by Government owned clinics would involve billions in Government expenditure, a total restructuring of the primary Healthcare system and lead to a less agile and responsive health care system. This outcome is possible, should the viability of General Practice be ignored.
General Practice is almost exclusively funded by fee for service income underwritten by Medicare which is, in essence, a Government funded Health Insurance Scheme.
Unfortunately, recent policies are discouraging effective primary care and leading to unintended downstream consequences. In fact, current policies are threatening the viability of General Practice. In real terms there has been a disinvestment in primary care. This is in stark contrast to Federal funding to other sectors such as 4.5% or more annual increase in investment in Pharmacy (4); 5% average increase in Private Health Insurance premiums underwritten by the Private Health Insurance Rebate (5); and an average ~ 5% p.a. increase in investment in State Health acute and hospital services (6).
Figure 2 Funding for GP has not kept pace with Health Inflation or with funding for other health areas. . Source: Dart, J 2020. Data sourced from (4) (5) (6) and Medicare
In contrast, the cost of providing General Practice has increased significantly. Practices employ staff, buy medical supplies such as equipment, dressings and PPE all of which and are subject to health specific inflation and which have significantly increased as a result of the pandemic.
Even before the pandemic, Government support was grossly deficient compared to the cost of providing General Practice care as shown in the graph below.
Figure 3 Medicare Indexation continues to diverge from the costs of providing healthcare. Source: RACGP News GP 7 July 2021 (from The Health of the Nation 2020)
This gap between the cost of providing Primary Healthcare and the funding from Medicare results in reduced income for GPs and therefore the reduced viability of General Practices. This means the (currently) small group of patients who are privately billed pay a larger “gap fee” to make up for reduced returns from bulk billing patients.
As a consequence of reduced GP incomes, the proportion of medical graduates selecting General Practice as a specialty is declining, and the declining viability of Practices is reducing the opportunity for effective succession planning, threatening generational change.
General Practice is now facing GP shortages in all areas of Australia from outer urban to regional and remote areas.
A Deloitte Access Economics General Practitioner Workforce Report 2019 produced for Cornerstone Health suggests that by 2030 the gap between the demand for GP services and the available supply of those services will in fact be most acute in outer urban areas rather than in regional and remote areas. The report suggests that by 2030 there will be:
- A 37.5% national increase in demand for GP services between 2019 and 2030
- A shortfall of 9298 full-time GPs or 24.7% of the GP workforce.
- Deficiency of GPs is expected to be most extreme in urban areas with a shortfall of 7,535 fulltime GPs or 31.7% by 2030.
RACGP Health of the Nation 2020 reports a fall in application rates for their Fellowship Program declining from 2458 applicants in 2015 to 1555 applicants for the 2022 intake.
Current Policies Discourage Managing Complexity in Primary Care
By not appropriately indexing Medicare, policy settings have driven practitioners to shorter, lower value, higher volume care.
Although the Medicare Benefits Schedule p28 states that “The fee for any item listed in the MBS is that which is regarded as being reasonable on average for that service having regard to usual and reasonable variations”, the scheduled fee had not been indexed between 2013-2019 and has been inappropriately indexed at no greater than 1.6%. This is a real de-funding of primary care.
The current rebate structure creates financial disincentives for complex care and encourages high volume, low value consultations which result in higher downstream costs in terms of unnecessary testing (radiology and pathology), unnecessary prescriptions (often antibiotic) and avoidable hospitalisations. The declining viability of Practices has seen the rise of corporate structures focussing heavily on short consultations.
Figure 4 Diminishing returns promote shorter, poor value consultations Source: RACGP 2020
To use an analogy – current policy settings focus on resourcing the ambulance at the bottom of the cliff rather than building safer roads.
It is well known that longer consultations with a regular GP avoid many of these downstream costs. Any associated costs will be more than accounted for by downstream savings.
A blended payment model which retains fee for service and increased funding for complex care may support more complex care models. However, a system without fee for service will not remain viable, will lead to unrestrained demand on the healthcare system, clinician burnout and an exodus of GPs as has been witnessed in the NHS.
Similarly, while blended payments are well suited to the management of chronic conditions, the fee for service approach and the ability to move between practices easily has been an essential part of the ease of access and accordingly patient equity for acute issues. Accordingly it needs to be retained for episodic care.
Without significant investment, Primary Care in Australia will suffer and the quality of primary care available to Australians will inevitably decline. Australia has an enviable reputation for the equity of access to high quality primary care. It is essential that policy decisions which threaten access to primary care are reversed and that future policy settings seek to maintain access and high quality primary care.
References
- Australian Bureau of Statistics. Patient experiences in Australia: Summary of findings, 2016–17. ABS cat. no. 4893.0. Canberra: ABS, 2017. Available at www.abs.gov.au/ ausstats/abs@.nsf/mf/4839.0 [Accessed 9 August 2018].
- Department of Health. Annual Medicare statistics: Financial year 1984–85 to 2017– 18. Canberra: DoH, 2018. Available at www.health.gov.au/internet/main/publishing. nsf/content/annual-medicare-statistics [Accessed
17 August 2018]. - The Royal Australian College of General Practitioners. General Practice: Health of the Nation 2018. East Melbourne, Vic: RACGP, 2018.
- Reserve Bank of Australia, 2018. Chapter 4 Inflation, accessed 29 March 2019, available at https://www.rba.gov.au/publications/smp/2018/aug/pdf/04-inflation.pdf
- Dunlevy, S 2015. It will take seven years of your taxes to pay off this $117000 pay rise granted by the Government, accessed 17 March 2019, https://www.news.com.au/lifestyle/health/health-problems/it-will-take-seven-years- of-your-taxes-to-pay-off-this-117000-pay-rise-granted-by-the-government/news- story/ee1743b2ea55913c5614bf6755af233d
- Savage, E, 2016. Is a 5.6% increase in Private Health Insurance Premiums justified?, accessed 17 March 2019, https://theconversation.com/is-a-5-6-increase-in-private- health-insurance-premiums-justified-55435
- The Department of Health, 2019. National Health Reform Funding, access 17 March 2019, http://www.health.gov.au/internet/main/publishing.nsf/Content/public-hospitals
- Hogne Sandvik, Øystein Hetlevik, Jesper Blinkenberg and Steinar Hunskaar. “Continuity in general practice as predictor of mortality, acute hospitalisation, and use of out-of-hours care: a registry-based observational study in Norway“ British Journal of General Practice 4 October 2021; BJGP.2021.0340.